Primitive Reflex Integration Case Studies
Preschooler Overcomes Selective Mutism with Reflex Integration
SLP uses neurodevelopmental movements to transform selective mutism while also helping with anxiety, toilet-training, and fine motor issues
This preschool girl with selective mutism only spoke to family members, needed to be in control, and at nearly 5 years of age was still wearing pull-ups and refusing to potty-train. Her SLP began incorporating rhythmic movements and reflex integration from the Brain and Sensory Foundations course into their therapy sessions, and saw immense changes: Her client now speaks to classmates and people she’s just met, she’s fully toilet-trained, and her fine motor skills have progressed substantially—see her drawings below.
Submitted by Carrie Eskenazi, MS, CCC-SLP

| Before | After |
|---|---|
| Selectively mute around anyone who was not a family member | Joining activities with others at school, talking with classmates, and even speaking to children she doesn't know at the park and other non-home environments |
| Still wearing pull-ups and not using the toilet at all | Wearing underwear 24/7, using the toilet, and dry at night |
| Unable to independently cross midline, demonstrated poor balance, unable to sit still for more than a few seconds | More able to control her body in a predictable and organized way |
| Drawings consisted of simple shapes representing objects and people; light strokes | Drawing is much improved, with clearly defined objects and people; confident strokes |
[Email communication to Sonia Story on 10/23/25]
Hello Sonia,
I wanted to share a story with you about a client who is finishing therapy with me this week because she no longer needs my support.
When she came to me she was 4 years, 10 months old and her parents were very concerned because she was selectively mute around anyone who was not a family member. In addition, she was still wearing pull-ups and not using the toilet at all. I did a speech-language evaluation and her language skills were above average. She had just a few misarticulations in her speech, but nothing that would interfere with her being understood. She liked to be in control and she told her mom, "I'll use the potty when I'm ready".
Here's the definition of Selective Mutism that I was working with [combined from different sources*]:
Selective mutism is a social anxiety disorder characterized by a consistent inability to speak in specific social situations, such as school or public settings, despite being able to speak comfortably in other familiar environments. It is not a choice or a behavior problem, but rather a manifestation of anxiety. Factors contributing to selective mutism can vary from person to person, but common factors include genetic predisposition, temperament, and environmental influences. It is important for students with selective mutism to receive appropriate support in order to facilitate development of academic and social emotional skills, which will allow them to participate in the classroom, access their school curriculum and form friendships.
What was important for me as a clinician was to discover the "why" of the anxiety. For this young girl, I believe it was partially or even mostly due to her underdeveloped sensory system. I don't think her body felt reliable or "safe", so I think she was reserving her resources and attempting to control her environment.
When I did a sensory assessment, I found that she had not yet differentiated head and eye movement, she was unable to converge her eyes, she was unable to independently cross midline, her balance was poor, she was unable to sit still for more than a few seconds, and she demonstrated overflow in her arms, hands, and mouth with motor activities. She had many unintegrated primitive reflexes, including Spinal Galant, Tonic Labyrinthine Reflex, Symmetrical Tonic Neck Reflex, Asymmetrical Tonic Neck Reflex, Fear Paralysis Reflex, and Moro; plus several underdeveloped postural reflexes.
We started right away with rhythmic movements [from the Brain and Sensory Foundations course] during sessions and at home. We began moving through reflexes as her brain/body became more organized. The cognitive side of therapy consisted mostly of visuals and talking about age appropriate social situations/skills. We also talked about sitting on the toilet, underwear and related topics. We focused on scaffolding skills with very small and doable changes, which would increase the difficulty level only slightly. We made sure she agreed with each change.
Over 10 months, she went from saying nothing to non-family members to joining activities with others at school and talking with school mates. She now talks to children she doesn't know at the park and other non-home environments. She wears underwear 24/7, uses the toilet, and is dry at night. She is still "shy", but she understands that she can choose to use her voice when she wants to and that her body is working for her in a more predictable and organized way. I've talked with you before about seeing children "arrive" in their bodies and I definitely observed this phenomenon several months ago with this child.
All of this is to say that, once again, I see the power of the movement work you've taught me and I am so grateful that I can give this gift to others.
I've attached her drawings of a person, house, and tree from when she first came to me (Dec. 2024), 5 months later, and 10 months later.
Warmly,
Carrie Eskenazi, MS, CCC-SLP
A progression of improvement—On each date, this child was requested to draw a person, a house, and a tree.
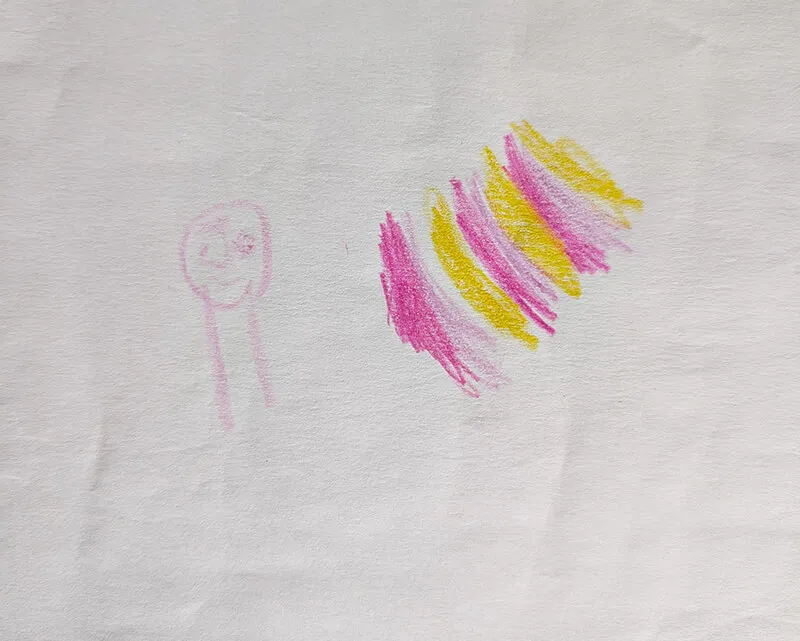
December 22, 2024

May 22, 2025

October 22, 2025
*Sources:
Selective Mutism Association [selectivemutism.org/what-is-sm/]
Helping Your Child with Selective Mutism, Angela E. McHolm, Ph.D., Charles E Cunningham, Ph.D., Melanie K Vanier, MA., New Harbinger Publications, Inc., 2006
*Disclaimer: The activities in the Brain and Sensory Foundations curriculum make use of the natural processes of neuroplasticity and development that are innately wired in the design of human beings to promote maturity and function. These activities appear to calm, organize, and mature the neuro-sensory-motor systems just as we see in the healthy development of human infants. Individual results may vary, and we do not claim to offer a diagnosis or cure for any specific condition or disorder. The Brain and Sensory Foundations activities appear to improve overall functioning resulting in measurable improvements for a range of conditions as demonstrated in over 1800 case studies from participants.

