Page Not Found
The page you requested is not available or has moved.
See popular, inspiring, and useful articles:
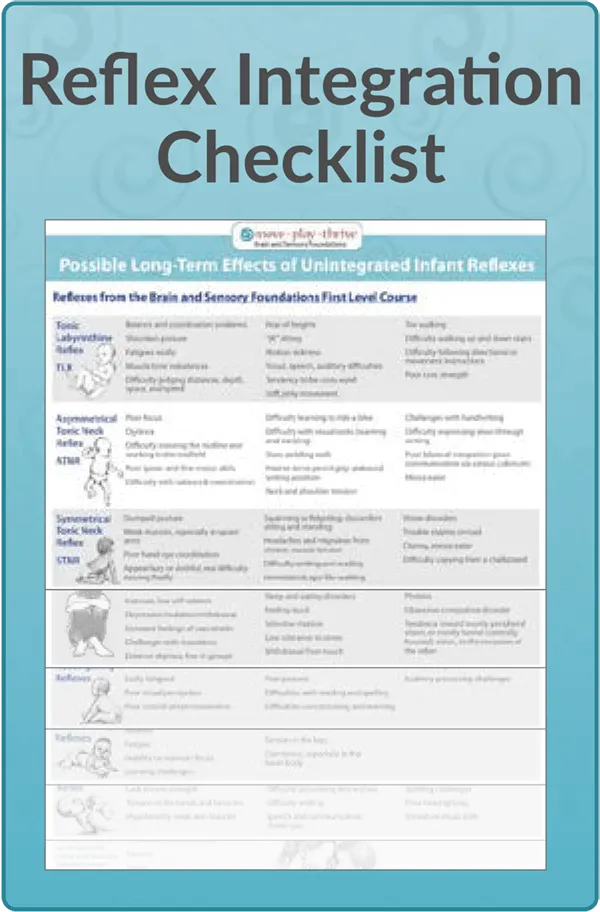
- Our unique Primitive Reflex Integration Continuing Education Course
- Addressing Challenging Conditions with Primitive Reflex Integration
- The Importance of Reflex Integration
- What is Rhythmic Movement Training?
- Outstanding Case Studies from Professionals and Parents